Endometrial Cancer Statistics
First, some statistics. Endometrial cancer is the most prevalent of the gynecological cancers. The American Cancer Society expect about 67,880 new cases of cancer of the uterus to be diagnosed in 2024. The death rate from all uterine cancers is projected to be 13,250 women.
Women of post menopausal age are most likely to be diagnosed with endometrial cancer with the average age of diagnosis being 60. Incidence rates continue to increase 1% in white women and about 2-3% per year in other racial/ethnic groups. Of further concern is the fact that this cancer is one of the few where increased mortality is seen with an increase of approximately 1.7% per year. In addition, endometrial cancer is very underfunded in comparison to other gynecological cancers. Limitations in funding produce limited research.
Survival Rates
Five year survival rates for endometrial cancer are as follows:
- Localized 95% (within the uterus only)
- Regional 70% (uterus and related areas such as ovaries or fallopian tubes)
- Distant 18% (uterus and unrelated organs)
- All stages combined 81% survival rate.
These numbers do not mention projected outcomes for dedifferentiated endometrial carcinoma. It would appear that this is a result of the rarity of this particular cancer as well as its being a relative newcomer. The closest numbers that one can extrapolate from are for undifferentiated endometrial cancer and those numbers aren’t all that encouraging. The stage of the cancer correlates to the survival rate. The five year survival rate is something like 57% with each increase in stage showing 15-20% decrease in survival rates. Recently approved immunotherapies may improve these statistics.
So What is Endometrial Cancer?
Now that I’ve presented some of the depressing facts, let’s move on to discuss what endometrial cancer is. Endometrial cancer is a cancer of the interior lining of the uterus. It is a uterine cancer but not the only one. Endometrial cancer accounts for approximately 90% of uterine cancers. Uterine sarcoma, a malignant tumor forming in the muscles or connective tissue of the uterus, makes up the other 10% of uterine cancers. We will be dealing here primarily with endometrial cancer.
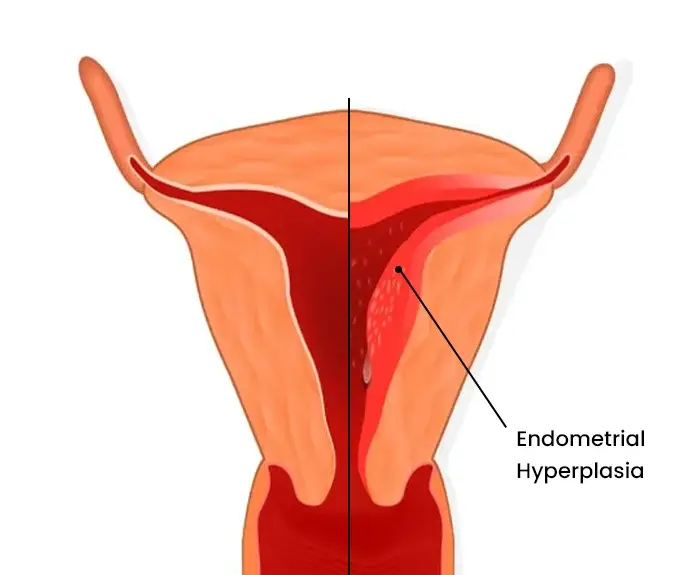
Endometrial Hyperplasia
Endometrial hyperplasia is a thickening of the endometrial lining of the uterus and is the precursor to cancer. It is not cancerous in and of itself but often leads to cancer.
The most common symptom of endometrial hyperplasia or endometrial cancer is abnormal bleeding. With the average age of diagnosis being 60 years old, most women are well into menopause. Any bleeding is concerning and should be brought to the attention of a gynecologist for evaluation. It gets more difficult when a woman who is still menstruating bleeds excessively since there are a variety of reasons that might be the case. Nevertheless, excessive bleeding should always be cause for concern and examination by your gynecologist.
Cause of Endometrial Hyperplasia
What causes endometrial hyperplasia? The primary trigger is estrogen. While there can be several reasons for estrogen increases, the primary one is obesity. Another possibility is hormone replacement therapy.
Trans vaginal ultrasound can measure the thickness of the uterine lining allowing for the diagnosis of endometrial hyperplasia. It is a simple test that requires a full bladder which is the most uncomfortable part of the test. Thickness less than 5mm generally rules out endometrial hyperplasia.
Endometrial Biopsy
A diagnosis of endometrial hyperplasia requires a biopsy to determine if malignancy is present. A biopsy, most often done in the office, uses a pipelle to obtain a tissue sample from the endometrium. Unfortunately, for some women, biopsies can be painful. Results are not always accurate since the pipelle scraping can miss the tumor site and give a false negative.
Another method of getting a endometrial sample includes a dilation and curretage (D&C) and a hysteroscopy. A D&C requires sedation. The physician is able to scrape a larger sample of tissue using this method. A hysteroscopy uses a camera and allows the doctor to visualize the endometrium and take samples as needed.
Diagnosis
At this time the pathologist is able to assess the sample and will determine if there is a malignancy or not. The grading of that sample takes into account the type of endometrial cancer and how aggressive it is. The grading system for endometrial cancer ranges from grade 1 – 3 with 3 being the most aggressive.
Types of Endometrial Cancer
The least aggressive, most common endometrial cancer is endometroid adenocarcinoma, usually grade 1 and due to estrogen and secondary to endometrial hyperplasia. Type 1 cancer is most often found in post menopausal women.
Type 2 is called clear cell, serous carcinoma. There is no precursor and this is more aggressive and occurs, usually, in much older women. Since it is more aggressive, this is either a grade 2 or 3.
Undifferentiated or dedifferentiated endometrial carcinomas are often not mentioned. Both of these are extremely aggressive and much more rare than the above mentioned types. Dedifferentiated is considered the most aggressive of the bunch since it is actually two endometrial cancers in one.
Treatment Options
Treatment for all varieties follows a similar path. Hysterectomy is the usual solution, believing that removal of the source is necessary. With stage 1, grade 1 diagnoses, intervention often stops there. For cancers diagnosed with a higher stage or grade, chemotherapy, radiation, or both are standard of care.
I just recently found a fabulous Youtube video on this very topic. This video is a great starting point for understanding endometrial cancer.